What You Should Know about Pfizer’s and Moderna’s COVID-19 Vaccine and Allergies
CONNECT WITH US:
Don’t Freak Out – It’s Not as Bad as You Think
On December 11, 2020 the U.S. Food and Drug Administration issued the first emergency use authorization of the coronavirus disease 2019 or COVID-19 vaccination. Since distributing the vaccine to healthcare workers across the U.S. there have been reports, such as the two health care workers in Alaska, of people developing concerning allergic reactions after receiving the vaccine.
As a Board-Certified Allergist and Immunologist with over twenty years of experience, I want to shed some light on the misinformation spreading about the use of this new vaccine in allergic patients.

Real Hope on the Horizon
The Pfizer-BioNTech vaccine is being reported as 95% effective – this is an astounding result, which should give all of us great hope that this coronavirus pandemic will end in the near future. It’s unprecedented that a vaccine went from the laboratory to being administered in less than a year. In fact, vaccine development typically takes 10-15 years on average with multiple vaccine trials before getting approval. Kudos to all the great scientists that contributed to this outstanding effort.
Public Concerns
There are many concerns and fears the public has about this new vaccine: will it really protect them? Is it safe? Will there be any short-term or long-term side effects? Can this give them the virus?
The available evidence points to many positive findings: the vaccine, as mentioned, appears to be very effective when administered as 2 doses given 3 weeks apart. In the over 40,000 doses given so far, the vaccine appears to be very safe. There were reported adverse reactions, mainly typical ones associated with vaccines like shingles: body aches, low-grade fever, injection site pain, and fatigue. These typically resolved within 24 hours.
Allergic Reaction to the Vaccine
Since starting the administration of the vaccine, The New York Times, USA Today other news outlets reported a handful of allergic reactions to the vaccination. But this is a handful out of the almost 5 million doses administered to date with almost 2 million administered in the U.S.
Two patients in England, both healthcare workers, reported having an anaphylactic reaction to the Pfizer vaccine. Both patients had a history of severe food allergy and carried epinephrine injectors for these exposures. These reactions set off the first wave of anxiety among anyone that has a history of an allergic reaction. On December 28th, a Boston Medical Center doctor, Dr. Hossein Sadrzadeh who has a severe shellfish allergy, said he had an allergic reaction to the Moderna vaccine within moments of receiving the first dose of the vaccine. He is the first person to have a known allergic reaction to Moderna’s coronavirus vaccine. More than 35,000 people have gotten the vaccine already in Massachusetts.
As a result of the reactions, British regulators advised those with severe allergies to avoid the vaccine. The U.S. trials of the vaccine kept out subjects who have had severe allergic reactions even though the vaccine does not contain preservatives or egg products, which have been known to trigger reactions with other types of vaccines.
U.S. health officials say both Moderna’s and Pfizer’s coronavirus vaccines are safe and medical experts agree that allergic reactions from vaccines are rare.
Given the handful of allergic reactions so far, it was reported that anyone with allergies should avoid the vaccine – this is not true!
Adverse Reactions vs. Anaphylactic (Severe Allergic Reactions) to Vaccines
Adverse reactions can be local or generalized. They result from the vaccine stimulating an immune response – which is typically a good thing. It’s unpleasant to have a sore arm, a fever, or muscle aches but this clearly means the immune system is engaging with the vaccine. Many people are fortunate that this immune response happens more subtly and they don’t experience any noticeable reaction after receiving the vaccine.
Anaphylactic reactions to vaccines are exceedingly rare but have occurred with vaccines. Pfizer states that there is a remote chance that the vaccine could cause a severe allergic reaction to the vaccine.
The typical vaccination concerns in the past were patients with a serious food allergy to eggs, as the measles vaccine and some others are incubated in egg embryos to produce. Another ingredient in vaccines that can cause an allergic reaction are gelatin; this is a substance to preserve the virus but contains either pulverized pork or fish – so someone allergic to these foods can potentially have an allergic reaction. Another ingredient that has been taken out of many vaccines was thimerosal; a preservative that contained some mercury and was known to trigger allergic reactions in patients with a mercury allergy (it was also common in contact lens solutions).
The key point: the Pfizer vaccine and Moderna vaccines don’t include any of these ingredients. The vaccines are made up of messenger RNA in a lipid nanoparticle covering, sucrose( a sugar) and use polyethylene glycol as a stabilizer in the lipid bubble to protect the messenger RNA from being dissolved before it enters our cells. Although it is unclear at this time, there is a high suspicion that the polyethylene glycol may be the cause of the anaphylactic reactions; it has a history of being the surreptitious agent in several medicines and injections that can cause these severe allergic reaction.
What Should a Person with Allergies Do?
It’s complicated and I would strongly urge any patient with allergies to discuss this issue with their doctor or their allergist.
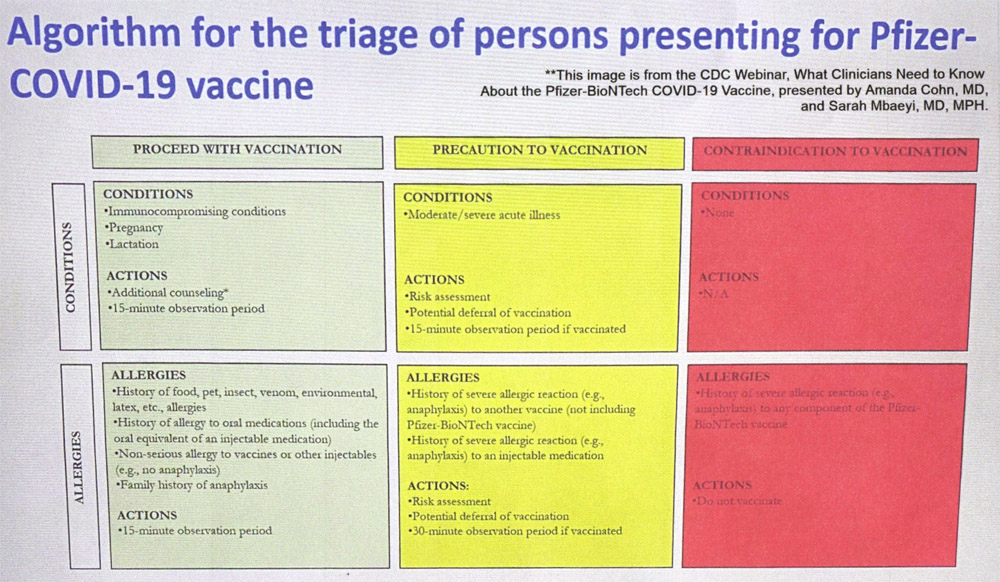
The CDC has provided an algorithm with guidelines what they believe is the appropriate risk for allergic patients. It should be noted the European Union’s guidelines have different criteria and have actually issued recommendations that anyone with an anaphylactic reaction to a food, medicine, or vaccine delay vaccination.
Please see the algorithm below – Algorithm for the triage of persons presenting for Pfizer-COVID-19 vaccine – that clearly divides vaccination precautions into 3 categories: green, yellow and red.
Note, the green column includes people with food, pet, venom, environmental or latex allergies are not to be excluded from receiving the vaccine. There does not appear to be any correlation with one of these specific allergens and a reaction to COVID-19 vaccine.
More caution should be advised in any person with a history of anaphylaxis to an injectable medicine; there is no known mechanism to explain this however, these patients are in the yellow column. This means they can receive a vaccination but in an experienced facility such as a hospital or doctor’s office – not a pharmacy – and wait 30 minutes following the vaccination to be observed.
The red column that notes a contradiction to the vaccine seems to be more of a medical-legal issue. It basically is saying if you have received the initial dose of the vaccine and you had an anaphylactic reaction you should not receive the 2nd dose: makes sense.
Final Thoughts
We are all going through this difficult time; but as history has shown us with polio and other dangerous infectious diseases, vaccinations are the way to making the public safer and return to our normal way of life.
My concern as an allergist and having cared for thousands of allergic patients I do have reservations about highly allergic patients receiving the vaccine at this time. Many highly allergic patients tend to have over-reactive mast cells which can be triggered to release massive amounts of histamine if activated. It is unclear what always causes this activation, but any type of inflammation-even from a vaccine- is possible.
Discuss your concerns with your doctor or an allergy specialist if you still have questions.
About the Author – Dr. Dean Mitchell, M.D.
Dr. Dean Mitchell M.D. is a Board-Certified and Immunologist based out of NYC. He graduated from the Sackler School of Medicine and completed training at the Robert Cooke Allergy Institute in New York City. He is also a Professor of Clinical Immunology at Touro College of Osteopathic Medicine, a fellow of the American Academy of Allergy, Asthma and Immunology, and the author of Allergy and Asthma Solution: The Ultimate Program for Reversing Your Symptoms One Drop at a Time. Dr. Dean Mitchell, M.D. has also been featured in The New York Times, The Huffington Post, Fitness Magazine, Dr. Oz and News NY 1. Dr. Mitchell also hosts the podcast The Smartest Doctor in the Room – a combination of a lively, personal, and in-depth interview with top healthcare specialists.
★ CONNECT WITH DR. MITCHELL ★
ADDITIONAL REFERENCES
- What’s in the Pfizer and Moderna COVID-19 Vaccines? Experts Explain the Ingredients
- Sellatura P, Nasser S and Ewan P. Polyethylene Glycol-Induced Systemic Allergic Reactions(Anaphylaxis). J Allergy Clin Immunol Pract month 2020: 1-6.
- The New York Times, December 19th, 2020. What You Need to Know About the Vaccines and Allergies, pg A11.